Pressure Ulcers (Bedsores): A pressure injury refers to the damage or impairment of skin integrity. It occurs when skin and underlying tissue are compressed between a bony prominence and an external surface for an extended period.
- Tissue compression can lead to: (Pressure ulcer prevention and management notes for AIIMS NORCET)
- Restricted blood flow causing ischemia.
- Inflammation and necrosis.
- Pressure injuries are difficult to heal once they develop.
Pressure Ulcers (Bedsores): Symptoms, Staging, and Optimal Care Strategies
Risk Factors
- Skin pressure: Prolonged application of pressure on skin.
- Shearing and friction: Movement causing skin damage.
- Immobility: Limited movement increases pressure injury risk.
- Malnutrition: Inadequate nutrition slows skin healing.
- Incontinence: Constant moisture weakens skin.
- Decreased sensory perception: Reduced ability to detect discomfort and pressure.
How to prevent pressure ulcers in bedridden patients
- Preventing skin breakdown is a primary nursing role.
- Important steps:
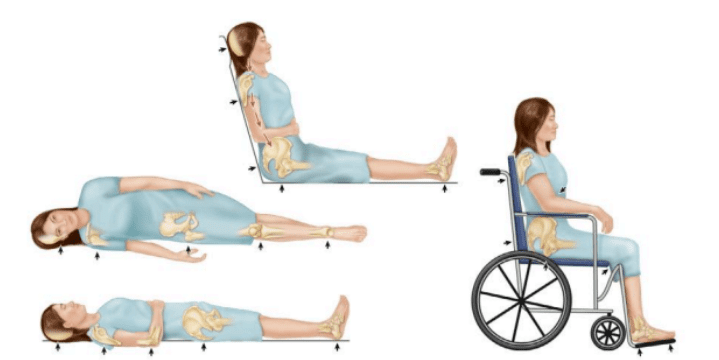
- Positioning: Ensure proper body alignment and use of pressure-relief devices.
- Skin cleansing and care: Regularly clean and care for the skin.
- Nutrition: Provide adequate nutrients for skin health.
- Moisture management: Use barrier creams for incontinent clients.
Pressure Ulcers (Bedsores) Interventions
- Avoid massage on reddened areas as it may damage capillary beds and worsen tissue necrosis.
- Identify high-risk clients: Monitor their skin closely.
- Frequent repositioning: Turn immobile clients every 2 hours and perform range-of-motion exercises at least every 8 hours.
- Skin maintenance:
- Keep skin dry and sheets wrinkle-free.
- Immediately change soiled pads or items under the client.
- Use lubricating creams and barrier ointments for protection.
- Monitor skin integrity: Perform regular assessments to detect early signs of breakdown.
Management of Pressure Injuries
- Documentation of Pressure Injuries
- Record the location and size of the wound (length, width, depth in centimeters).
- Monitor and document the type and amount of exudates (e.g., serosanguineous or purulent).
- Assess for undermining (separation of tissue under wound edges) and tunneling (channels extending into surrounding tissue).
- Include picture documentation (with client identifier, measuring device, wound laterality, and location) as per agency protocols.
- Refer to a wound care or nutrition specialist if required.
- Exudate Analysis
- Serosanguineous exudate: Pale, pink, and watery; typically normal.
- Purulent exudate: Yellow, green, or tan; indicates bacterial colonization and infection.
- Adherence to Protocols
- Follow agency protocols for wound management and skin integrity assessment.
- Treatment Options
- Wound dressings and debridement: Removes dead tissue to promote healing.
- Skin grafting: May be necessary for severe injuries.
- Advanced Treatments
- Electrical stimulation: Stimulates blood vessel growth and granulation tissue formation.
- Vacuum-assisted wound closure: Removes infectious material and promotes granulation.
- Hyperbaric oxygen therapy: Provides oxygen under high pressure to enhance tissue oxygenation.
- Topical growth factors: Biologically active substances that stimulate cell growth.
Pressure Ulcers (Bedsores) Types of Exudate from Wounds
- Serous Exudate
- Appearance: Clear or straw-colored and watery.
- Indication: Typically associated with the inflammatory phase of healing and represents normal wound drainage.
- Serosanguineous Exudate
- Appearance: Pale pink and watery.
- Indication: Indicates a mix of serous fluid and blood, often seen in wounds healing normally.
- Sanguineous Exudate
- Appearance: Bright red drainage.
- Indication: Abnormal sign indicating active bleeding, which may require immediate medical attention.
- Purulent Exudate
- Appearance: Yellow, gray, tan, brown, or green in color.
- Indication: Suggests the presence of infection in the wound, often accompanied by an unpleasant odor and inflammation.
Key Points to Remember:
- Serous and serosanguineous exudates are generally normal during wound healing.
- Sanguineous and purulent exudates may indicate complications like bleeding or infection, requiring prompt intervention.
- Always assess the amount, color, odor, and consistency of wound exudate for effective wound management.
Stages of Pressure Injuries –
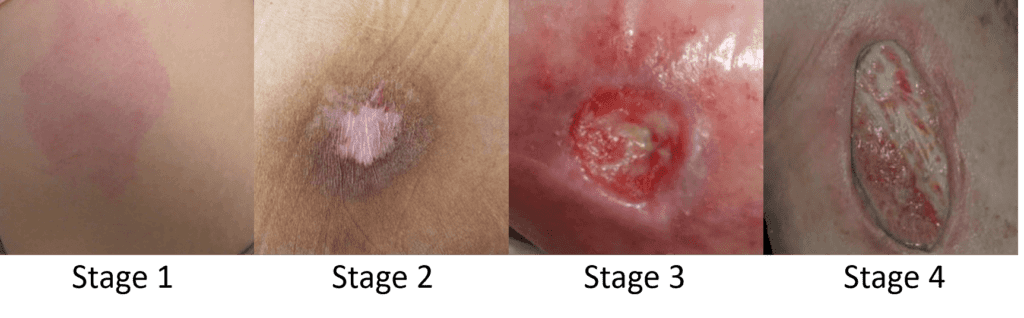
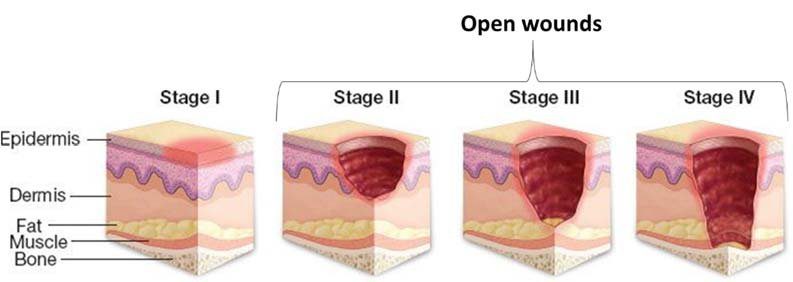
Stage 1: Non-Blanchable Erythema
- Description: Skin is intact with redness that does not blanch when pressure is applied.
- Key Features:
- May appear as different shades in darker skin tones.
- Often accompanied by changes in sensation, temperature, or firmness of the skin.
Stage 2: Partial-Thickness Skin Loss
- Description: Involves the loss of the outer skin layer (epidermis) and possibly the dermis.
- Key Features:
- Wound bed appears pink, red, and moist.
- May present as an intact or ruptured serum-filled blister.
Stage 3: Full-Thickness Skin Loss
- Description: Loss of skin down to the adipose (fat) tissue, but does not expose muscle, bone, or tendons.
- Key Features:
- Granulation tissue and rolled wound edges may be visible.
- Slough or eschar could be present.
- Undermining or tunneling may be noted.
Stage 4: Full-Thickness Tissue Loss
- Description: Extensive damage with exposure of muscle, tendon, ligament, cartilage, or bone.
- Key Features:
- Slough or eschar may cover parts of the wound.
- Undermining or tunneling could also be present.
Unstageable Pressure Injury
- Description: Full-thickness skin and tissue loss, but the extent cannot be determined due to coverage by slough or eschar.
- Key Features:
- Assessment of depth is not possible until slough or eschar is removed.
Suspected Deep Tissue Injury
- Description: Persistent non-blanchable discoloration of deep red, maroon, or purple.
- Key Features:
- May appear as a blood-filled blister or have epidermal separation.
- Common in darker skin tones where discoloration might be less noticeable.
Types of Dressings and Their Mechanisms of Action for Pressure Injuries
Stage 1 Pressure Injuries
- Dressing Type:
- None
- Transparent dressing
- Hydrocolloid dressing
- Mechanism of Action:
- Promotes slow resolution of redness without epidermal loss within 7 to 14 days.
Stage 2 Pressure Injuries
- Dressing Type:
- Composite film
- Hydrocolloid
- Hydrogel covered with foam or gauze dressing
- Mechanism of Action:
- Facilitates healing through reepithelialization.
Stage 3 Pressure Injuries
- Dressing Type:
- Hydrocolloid
- Hydrogel covered with foam dressing
- Calcium alginate
- Gauze
- Mechanism of Action:
- Promotes healing through granulation and reepithelialization.
Stage 4 Pressure Injuries
- Dressing Type:
- Hydrogel covered with foam dressing
- Calcium alginate
- Gauze
- Mechanism of Action:
- Assists in healing through granulation, reepithelialization, and scar tissue development.
Unstageable Pressure Injuries
- Dressing Type:
- Adherent film
- Gauze with a prescribed solution
- Enzymes
- Mechanism of Action:
- Eschar loosens and lifts at edges as healing progresses. Surgical debridement may be required.
Suspected Deep-Tissue Injury
- Dressing Type:
- Calcium alginate or others
- Mechanism of Action:
- Healing depends on the type of treatment used.
Adhesive Transparent Film
- Indications, Uses, and Considerations:
- Provides protection for partial-thickness lesions and debridement.
- Serves as a secondary (cover) dressing.
- Allows for good wound visualization.
- Waterproof and reduces pain.
- Best for superficial lesions.
- Nonabsorbent; adheres to normal and healing tissue, which may make it difficult to apply.
- Frequency of Dressing Changes:
- Change when leakage of exudates occurs.
- For necrotic base: Replace every 24 hours.
Superabsorbent Dressing
- Indications, Uses, and Considerations:
- Minimizes adherence to the wound while efficiently collecting exudate.
- Ideal for heavily exuding pressure injuries.
- Frequency of Dressing Changes:
- As often as necessary, depending on the saturation level with exudate.
Top 10 MCQs on Pressure Ulcers
Q1. What is the primary cause of pressure ulcers?
A) Inadequate nutrition
B) Pressure and shearing forces
C) Bacterial infection
D) Poor hygiene
Answer: B
Rationale: Pressure ulcers are caused by prolonged pressure, shearing, and friction that compress blood flow to the skin and underlying tissues, leading to tissue damage.
Q2. Which stage of pressure ulcers is characterized by intact skin with non-blanchable redness?
A) Stage 1
B) Stage 2
C) Stage 3
D) Stage 4
Answer: A
Rationale: Stage 1 pressure ulcers are defined by intact skin with non-blanchable redness, indicating localized tissue damage.
Q3. In which stage of a pressure ulcer is subcutaneous tissue exposed with possible tunneling or undermining?
A) Stage 1
B) Stage 2
C) Stage 3
D) Stage 4
Answer: C
Rationale: Stage 3 pressure ulcers involve full-thickness tissue loss, exposing subcutaneous fat, with possible undermining or tunneling.
Q4. What is the most appropriate dressing for a Stage 1 pressure ulcer?
A) Hydrocolloid dressing
B) Transparent dressing
C) Calcium alginate
D) Hydrogel with foam
Answer: B
Rationale: Transparent dressings are suitable for Stage 1 ulcers to prevent further injury while allowing observation of the wound.
Q5. What is the first intervention for preventing pressure ulcers in immobile patients?
A) Use of hydrocolloid dressings
B) Repositioning every 2 hours
C) Applying lotion to the skin
D) Using calcium alginate dressings
Answer: B
Rationale: Regular repositioning reduces pressure on specific body areas, improving circulation and preventing ulcers.
Q6. Which of the following is a sign of a suspected deep-tissue injury?
A) Non-blanchable erythema
B) Persistent purple or maroon discoloration
C) Exposed muscle and bone
D) Ruptured serum-filled blister
Answer: B
Rationale: Suspected deep-tissue injuries are characterized by non-blanchable, deep red, maroon, or purple discoloration due to underlying tissue damage.
Q7. What is the recommended intervention for an unstageable pressure ulcer?
A) Applying transparent dressing
B) Surgical debridement of necrotic tissue
C) Using calcium alginate dressings
D) Moist wound healing with hydrogel
Answer: B
Rationale: Unstageable ulcers require debridement to remove necrotic tissue and allow proper wound assessment and healing.
Q8. Which of the following risk factors is most likely to contribute to the development of pressure ulcers?
A) High blood pressure
B) Decreased sensory perception
C) Smoking
D) High BMI
Answer: B
Rationale: Decreased sensory perception limits the ability to recognize and respond to pressure, increasing the risk of skin breakdown.
Q9. What type of exudate is indicative of wound infection?
A) Serous
B) Serosanguineous
C) Sanguineous
D) Purulent
Answer: D
Rationale: Purulent exudate, characterized by yellow, green, or brown drainage, is a sign of infection.
Q10. Which dressing type is most appropriate for heavily exuding Stage 4 pressure ulcers?
A) Hydrocolloid dressing
B) Transparent dressing
C) Calcium alginate
D) Enzymatic debriding agents
Answer: C
Rationale: Calcium alginate dressings are highly absorbent and suitable for wounds with heavy exudate, promoting granulation and healing.
Key Words
Pressure ulcer prevention and management notes for AIIMS NORCET, Important topics on bedsores for nursing officer exams, Pressure ulcers simplified: Study guide for nursing exams, AIIMS NORCET preparation: Pressure ulcers and their management, Key pressure ulcer topics for nursing competitive exams, Detailed notes on pressure ulcers for nursing officer exams, Stage-wise pressure ulcer treatment for AIIMS NORCET candidates, How to prepare for nursing exams: Focus on pressure ulcers, Pressure ulcer care tips for nursing officer exam preparation, Essential nursing notes on pressure ulcers for competitive exams
Best treatment options for stage 3 pressure ulcers, Early signs and symptoms of bedsores in elderly patients, Effective nursing interventions for pressure ulcer prevention, Why do pressure ulcers form, and how can they be avoided,

