Digestive System Notes for Nursing Officer Exam: The digestive system breaks down food into nutrients, absorbs them into the bloodstream, and eliminates waste products. Below is a step-by-step guide covering the digestive system’s structure, function, and physiological processes, organized in a way that’s easy for nursing officer exam preparation.
Digestive System Notes for Nursing Officer Exam
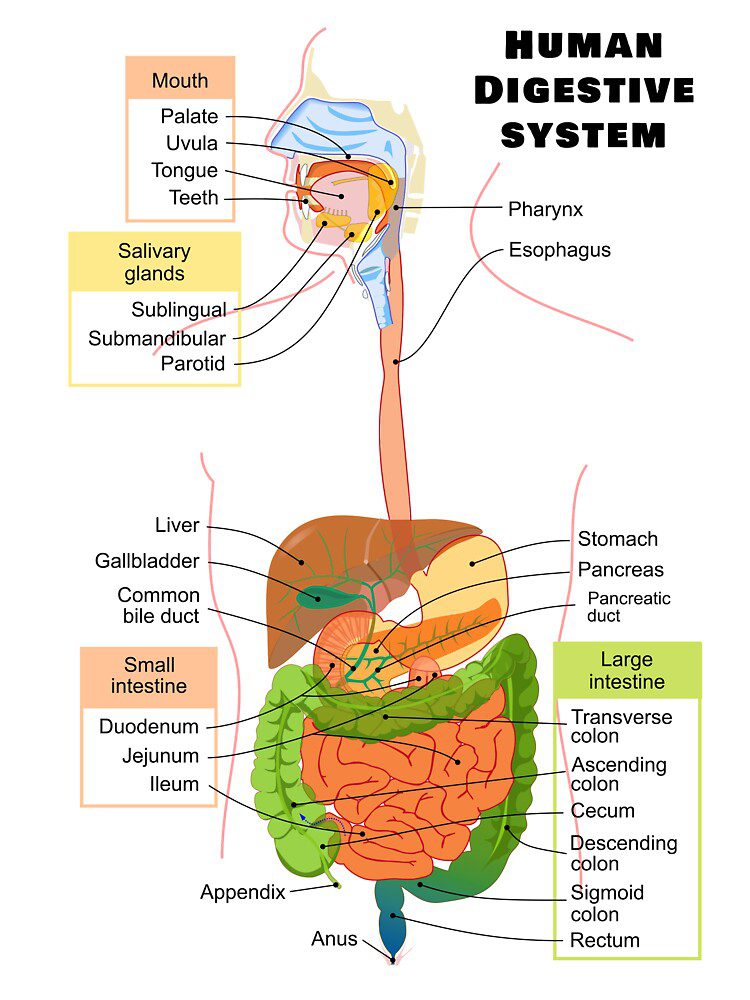
1. Overview of the Digestive System
- Definition: The digestive system processes food to extract nutrients and eliminate waste.
- Main Components:
- Alimentary Canal: Includes the mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus.
- Accessory Organs: Teeth, tongue, salivary glands, liver, gallbladder, and pancreas.
2. Functions of the Digestive System
- Ingestion: The intake of food and liquids.
- Propulsion: Movement of food through the digestive tract, including swallowing and peristalsis.
- Mechanical digestion: Physical breakdown of food (e.g., chewing and stomach churning).
- Chemical digestion: Breaking down food into simpler molecules by enzymes and acids.
- Absorption: Transporting digested nutrients into the bloodstream or lymphatic system.
- Defecation: Elimination of indigestible substances and waste.
3. Mouth (Oral Cavity)
- Structure:
- Teeth: Incisors, canines, premolars, and molars used for chewing.
- Tongue: Moves food and aids in the mixing process; contains taste buds.
- Salivary Glands: Secrete saliva containing amylase (breaks down starch).
- Function:
- Mechanical digestion through chewing.
- Chemical digestion begins with salivary amylase (carbohydrate digestion).
- Mastication: The process of chewing to form a bolus for easier swallowing.
4. Pharynx and Esophagus
- Pharynx:
- Passageway for food, liquid, and air.
- Swallowing: Voluntary and involuntary actions that move food from the mouth to the esophagus.
- Esophagus:
- A muscular tube that connects the pharynx to the stomach.
- Peristalsis: Wave-like muscular contractions that move food towards the stomach.
- Lower Esophageal Sphincter (LES): Prevents the backflow of stomach acid into the esophagus (acid reflux).
5. Stomach
- Structure:
- J-shaped, muscular organ located in the upper left abdomen.
- Divided into: Cardia, Fundus, Body, and Pylorus.
- Pyloric Sphincter: Controls the movement of chyme into the small intestine.
- Function:
- Mechanical digestion: Churning action mixes food with gastric juices.
- Chemical digestion: Gastric juices containing hydrochloric acid (HCl) and pepsin begin protein digestion.
- Mucus: Protects stomach lining from acid.
- Absorption: Limited (water, alcohol, and some drugs).
- Production of Intrinsic Factor: Required for vitamin B12 absorption.
6. Small Intestine
- Structure:
- Length: Approximately 6 meters in adults.
- Divided into three parts: Duodenum, Jejunum, and Ileum.
- Villi: Tiny projections in the inner lining that increase surface area for absorption.
- Function:
- Duodenum: Receives bile (from the liver) and pancreatic juice (from the pancreas) to aid digestion.
- Jejunum and Ileum: Primary sites for absorption of nutrients into the bloodstream via the villi.
- Digestive enzymes: Secreted by the pancreas (amylase, lipase, proteases) and bile emulsifies fats.
- Absorption: Nutrients like glucose, amino acids, fatty acids, vitamins, and minerals are absorbed here.
7. Liver and Gallbladder
- Liver:
- Largest gland in the body, located in the upper right abdomen.
- Functions:
- Produces bile which emulsifies fats for digestion and absorption.
- Detoxifies harmful substances (e.g., alcohol, drugs).
- Stores glycogen, vitamins, and iron.
- Converts excess glucose into glycogen for storage.
- Metabolizes proteins and synthesizes albumin and clotting factors.
- Gallbladder:
- Stores and concentrates bile produced by the liver.
- Releases bile into the duodenum via the common bile duct to aid fat digestion.
8. Pancreas
- Structure: Located behind the stomach, the pancreas is both an endocrine and exocrine gland.
- Exocrine Function:
- Secretes digestive enzymes (amylase, lipase, proteases) into the duodenum to break down carbohydrates, fats, and proteins.
- Bicarbonate ions neutralize stomach acid entering the small intestine.
- Endocrine Function:
- Secretes insulin and glucagon to regulate blood sugar levels.
9. Large Intestine
- Structure:
- Approximately 1.5 meters long, divided into the cecum, colon (ascending, transverse, descending, sigmoid), rectum, and anus.
- Function:
- Absorption of water and electrolytes (sodium, potassium).
- Formation and storage of feces.
- Bacterial fermentation of undigested carbohydrates and production of vitamins like vitamin K.
- Defecation: Elimination of undigested material and waste products through the anus.
10. Defecation Reflex
- Structure: The rectum stores fecal matter, which is eliminated through the anus.
- Defecation Process:
- Stretching of the rectum stimulates sensory receptors.
- This activates the defecation reflex, leading to the contraction of rectal muscles and relaxation of the anal sphincters.
- Voluntary control over the external anal sphincter allows for appropriate timing of defecation.
11. Physiological Control of Digestion
- Nervous System Control: The enteric nervous system coordinates peristalsis, enzyme secretion, and other digestive functions.
- Hormonal Control: Key hormones include:
- Gastrin: Stimulates gastric acid secretion and motility.
- Secretin: Stimulates the pancreas to release bicarbonate.
- Cholecystokinin (CCK): Stimulates the release of bile and pancreatic enzymes.
- Ghrelin: Stimulates appetite.
- Leptin: Regulates satiety.
12. Common Digestive Disorders
- Gastroesophageal Reflux Disease (GERD): Acid reflux from the stomach into the esophagus.
- Peptic Ulcers: Open sores in the stomach or duodenum due to H. pylori infection or prolonged NSAID use.
- Irritable Bowel Syndrome (IBS): A functional disorder causing abdominal pain, bloating, and irregular bowel movements.
- Celiac Disease: An autoimmune disorder where gluten damages the small intestine lining, impairing nutrient absorption.
- Hepatitis: Inflammation of the liver, commonly caused by viral infections (A, B, C).
- Cholecystitis: Inflammation of the gallbladder, often due to gallstones.
13. Key Points to Remember
- The small intestine is the primary site for nutrient absorption.
- Bile and pancreatic enzymes are crucial for digestion in the duodenum.
- The liver performs vital metabolic, detoxifying, and digestive functions.
- Peristalsis is the key mechanism for moving food through the digestive tract.
- Proper hydration and balanced diet play an essential role in digestive health.
- Mouth – Begins mechanical digestion through mastication and mixes food with saliva for chemical digestion.
- Salivary Glands – Secrete saliva containing amylase, which starts the breakdown of carbohydrates.
- Pharynx – Passageway for food from the mouth to the esophagus.
- Esophagus – Muscular tube that uses peristalsis to move food to the stomach.
- Lower Esophageal Sphincter – Prevents acid reflux by closing off the esophagus from the stomach.
- Stomach – Churns food and mixes it with gastric juices to create chyme.
- Gastric Juice – Contains hydrochloric acid and pepsinogen, aiding in protein digestion.
- Pepsinogen – Activated to pepsin in the stomach to digest proteins.
- Pyloric Sphincter – Controls the passage of chyme from the stomach into the small intestine.
- Small Intestine – Main site for nutrient absorption, divided into the duodenum, jejunum, and ileum.
- Duodenum – First part of the small intestine where major digestion occurs.
- Jejunum – Middle section of the small intestine primarily involved in nutrient absorption.
- Ileum – Last part of the small intestine, absorbs vitamin B12 and bile salts.
- Villi and Microvilli – Increase surface area in the small intestine for maximum absorption.
- Lacteals – Lymphatic vessels in the villi that absorb dietary fats.
- Pancreas – Produces digestive enzymes and bicarbonate to neutralize stomach acid.
- Trypsin – Pancreatic enzyme that digests proteins in the small intestine.
- Chymotrypsin – Pancreatic enzyme that splits proteins into smaller peptides.
- Amylase – Pancreatic enzyme that breaks down carbohydrates.
- Lipase – Pancreatic enzyme that breaks down fats into fatty acids and glycerol.
- Liver – Processes nutrients from the digestive tract and produces bile.
- Bile – Emulsifies fats in the small intestine, making them easier to digest.
- Gallbladder – Stores and concentrates bile, releasing it into the duodenum.
- Large Intestine – Absorbs water and electrolytes, forming and storing feces.
- Cecum – First part of the large intestine, connecting to the ileum.
- Appendix – Small, vestigial organ attached to the cecum.
- Colon – Major part of the large intestine, absorbing water and salts.
- Rectum – Stores feces before defecation.
- Anus – Final part of the digestive tract where feces exit the body.
- Peristalsis – Involuntary contractions that move food through the digestive tract.
- Segmentation – Contractions in the small intestine that mix chyme and increase absorption.
- Enteric Nervous System – Autonomous nervous system within the digestive tract.
- Mucosa – Innermost layer of the digestive tract containing glands and cells for secretion.
- Submucosa – Connective tissue layer housing blood vessels, nerves, and glands.
- Muscularis Externa – Layer of muscle responsible for peristalsis and segmentation.
- Serosa – Outermost layer of the digestive tract, providing protection.
- Gastrointestinal (GI) Tract – Entire channel from mouth to anus involved in digestion and absorption.
- Chyme – Semi-fluid mass of partly digested food expelled by the stomach into the duodenum.
- Gastric Emptying – Process by which the stomach contents are transferred to the small intestine.
- Enterohepatic Circulation – Recycling mechanism of bile salts between the liver and the small intestine.
- Brush Border Enzymes – Enzymes on the microvilli of the small intestine that finalize digestion.
- Intrinsic Factor – Glycoprotein vital for vitamin B12 absorption, secreted by the stomach.
- Hartmann’s Procedure – Surgical operation involving resection of the rectosigmoid colon.
- GERD (Gastroesophageal Reflux Disease) – Chronic acid reflux affecting the lower esophageal sphincter.
- Peptic Ulcers – Sores that develop on the lining of the stomach, small intestine, or esophagus.
- Crohn’s Disease – Inflammatory bowel disease affecting any part of the gastrointestinal tract.
- Ulcerative Colitis – Chronic inflammatory condition limited to the colon and rectum.
- Diverticulosis – Formation of small pouches in the walls of the digestive tract.
- Constipation – Difficulty in passing stools because of slow bowel movements.
- Diarrhea – Frequent, loose, or watery stools resulting from increased intestinal motility.
- Irritable Bowel Syndrome (IBS) – Functional disorder characterized by symptoms like bloating, pain, and irregular bowel movements.
- Lactose Intolerance – Inability to digest lactose due to deficiency of lactase enzyme.
- Celiac Disease – Autoimmune disorder where ingestion of gluten leads to damage in the small intestine.
- Gastrectomy – Surgical removal of all or part of the stomach.
- Stoma – Artificial opening created surgically for waste elimination (e.g., colostomy).
- Hepatitis – Inflammation of the liver often caused by viral infection.
- Cirrhosis – Chronic liver damage leading to scarring and liver failure.
- Portal Hypertension – Increased blood pressure within the portal venous system.
- Jaundice – Yellowing of the skin and eyes due to high bilirubin levels.
- Gallstones – Hardened deposits formed in the gallbladder.
- Cholecystitis – Inflammation of the gallbladder often due to gallstones.
- Pancreatitis – Inflammation of the pancreas that can disrupt its functions.
- Colonoscopy – Diagnostic procedure to examine the colon’s interior.
- Endoscopy – Procedure using a flexible tube to view the digestive tract.
- Biopsy – Procedure to remove a small sample of tissue for examination.
- Barium Swallow – X-ray imaging test using barium to visualize the esophagus and stomach.
- Magnetic Resonance Cholangiopancreatography (MRCP) – Imaging technique to view the bile and pancreatic ducts.
- Helicobacter pylori – Bacterium strongly associated with peptic ulcer disease.
- Probiotics – Beneficial bacteria promoting a healthy gut microbiome.
- Prebiotics – Non-digestible fibers that benefit gut bacteria.
- Fiber – Indigestible plant material that aids in digestion and prevents constipation.
- Enteral Nutrition – Providing nutrients directly into the gastrointestinal tract.
- Parenteral Nutrition – Delivering nutrients directly into the bloodstream, bypassing the digestive system.
- Bowel Sounds – Noises made by the movement of the intestines, indicative of digestive activity.
- Gastroparesis – Delayed gastric emptying due to impaired stomach muscles.
- Hepatomegaly – Enlargement of the liver often indicating liver disease.
- Splenomegaly – Enlargement of the spleen linked to various pathological conditions.
- Tenesmus – Persistent, painful urge to pass stools despite an empty colon.
- Hematemesis – Vomiting blood, indicative of upper GI bleeding.
- Melena – Black, tarry stools suggesting upper GI bleeding.
- Hematochezia – Passage of fresh blood per anus, usually indicating lower GI bleeding.
- Esophagogastroduodenoscopy (EGD) – Endoscopic examination of the esophagus, stomach, and duodenum.
- Capsule Endoscopy – Swallowable camera capsule allowing for visualization of the small intestine.
- Carbohydrate Digestion – Initiated in the mouth by salivary amylase and completed by pancreatic amylase and brush border enzymes.
- Protein Digestion – Started in the stomach by pepsin and continued in the small intestine by pancreatic enzymes and brush border peptidases.
- Fat Digestion – Emulsified by bile, hydrolyzed by pancreatic lipase, and absorbed as micelles.
- Absorption of Vitamins – Water-soluble vitamins absorbed directly into the bloodstream; fat-soluble vitamins require dietary fats for absorption.
- Electrolyte Transport – Primarily managed by ion channels and transporters in the intestinal epithelium.
- Fluid Balance – Approximately 9 liters of fluid enter the GI tract daily, with most reabsorbed by the intestines.
- Splanchnic Circulation – Blood flow to the stomach, spleen, pancreas, intestines, and liver.
- Hepatic Portal Vein – Carries nutrient-rich blood from the gastrointestinal tract to the liver.
- Kupffer Cells – Specialized macrophages in the liver involved in breaking down red blood cells and bacteria.
- Enterocytes – Absorptive cells lining the villi of the small intestine.
- Gastroenteritis – Inflammation of the stomach and intestines often caused by infection.
- Oral Rehydration Therapy – Treatment for dehydration using a solution of salts and sugars.
- Colon Cancer – Malignancy arising from the lining of the colon or rectum.
- Polyps – Benign growths on the lining of the colon that can become cancerous.
- Fecal Occult Blood Test (FOBT) – Detects hidden blood in stool, used for colorectal cancer screening.
- Ileostomy – Surgical diversion of the ileum to an abdominal stoma.
- Sigmoidoscopy – Visualization of the sigmoid colon using a flexible scope.
- Anorexia – Lack or loss of appetite for food.
- Cachexia – Extreme weight loss and muscle wasting, often seen in chronic disease.
- Steatorrhea – Fatty stools indicative of malabsorption.
- Dysphagia – Difficulty swallowing due to esophageal or neurological disorders.
- Achalasia – Failure of the lower esophageal sphincter to relax, impeding food passage.
- Barrett’s Esophagus – Metaplasia of the esophageal lining, precursor to esophageal cancer.
- Gastrocolic Reflex – Increased peristalsis of the colon following a meal.
- Micelle Formation – Step in fat digestion where bile salts surround fatty acids and monoglycerides.
- Enterotoxins – Toxins affecting the intestines, often leading to diarrhea.
- Proctitis – Inflammation of the rectum’s lining.
- Gastric Bypass – Surgical procedure for obesity where the stomach is divided and rearranged.
- Gastric Banding – Adjustable band placed around the upper part of the stomach to restrict food intake.
- Nissen Fundoplication – Surgical technique to treat GERD by wrapping the stomach around the esophagus.
- Pharmacological Therapy – Includes proton pump inhibitors, H2 blockers, antacids, and laxatives for various GI disorders.
- Gastrointestinal Motility – Contractions of the GI muscles to move and mix contents.
- Colorectal Surgery – Includes resection, anastomosis, and stoma creation for treating diseases.
- Nasogastric Tube – Inserted through the nose into the stomach for feeding or decompression.
- Gastrostomy Tube – Surgically placed tube for long-term enteral feeding.
- Total Parenteral Nutrition (TPN) – Complete nutritional support bypassing the GI tract.
- Prokinetic Agents – Drugs that enhance gastrointestinal motility.
- Antiemetics – Medications to reduce nausea and vomiting.
- Hepatic Encephalopathy – Decline in brain function due to severe liver disease.
- Ammonia – Byproduct of protein metabolism, detoxified by the liver.
- Primary Biliary Cholangitis – Chronic liver disease causing bile duct damage.
- Wilson’s Disease – Genetic disorder causing copper accumulation in tissues.
- Acute Cholecystitis – Sudden inflammation of the gallbladder, typically due to bile duct obstruction.
- Hemorrhoids – Swollen veins in the rectum or anus causing discomfort and bleeding.
- Hernia – Protrusion of an organ through the wall of the cavity containing it.
- Inguinal Hernia – Occurs when tissue protrudes through a weak spot in the groin muscles.
- BMI (Body Mass Index) – Simple calculation using height and weight to assess body fat.
- Hyperalimentation – Excessive nourishment via parenteral nutrition.
- Liver Function Tests (LFTs) – Blood tests measuring liver enzymes, bilirubin, and proteins.
- Insulin – Pancreatic hormone regulating blood glucose levels.
- Glucagon – Pancreatic hormone increasing blood glucose levels by promoting glycogen breakdown.
- Cushing’s Reflex – Physiological response to increased intracranial pressure causing increased blood pressure, bradycardia, and irregular respiration.
- Hepatic Transplantation – Surgical procedure to replace a diseased liver with a healthy donor liver.
- Jejunal Feeding – Enteral nutrition delivered directly into the jejunum.
- MALABSORPTION SYNDROME – Failure to fully absorb nutrients from the gastrointestinal tract.
- MECKEL’S DIVERTICULUM – Congenital anomaly of the small intestine causing potential complications.
- SBO (Small Bowel Obstruction) – Partial or complete blockage of the small intestine.
- Peritonitis – Inflammation of the peritoneum, typically due to infection.
- H. PYLORI TEST – Diagnostic test for Helicobacter pylori infection.
- LACTULOSE – Laxative used to treat constipation and hepatic encephalopathy.
- FRUCTOSE MALABSORPTION – Improper absorption of fructose causing digestive symptoms.
- BOWEL PREP – Cleansing of the intestines before diagnostic procedures.
- INTESTINAL ADHESIONS – Fibrous bands forming between tissues and organs post-surgery.
- BILIARY ATRESIA – Congenital absence or closure of bile ducts, leading to liver damage.
- RECTAL PROLAPSE – Protrusion of rectal tissue through the anus.
- CHOLEDOCHOLITHIASIS – Presence of gallstones in the common bile duct.
- COLON ANASTOMOSIS – Surgical connection between two parts of the colon.
- VISCERAL PAIN – Pain originating from the internal organs.
- DOUMULT ASTERIXIS – Flapping tremor of the hands often seen in hepatic encephalopathy.
- PARACENTESIS – Procedure to remove fluid from the peritoneal cavity.
- CHOLECYSTECTOMY – Surgical removal of the gallbladder.
- FAT-SOLUBLE VITAMINS – Includes vitamins A, D, E, K requiring fat for absorption.
- LAPAROTOMY – Surgical incision into the abdominal cavity.
- ILEOCECAL VALVE – Controls the flow from the ileum into the cecum and prevents backflow.
- PERNICIOUS ANEMIA – B12 deficiency due to lack of intrinsic factor.
- CONSTIPATION – Fecal retention causing hard, infrequent bowel movements.
Here’s a collection of 50 multiple-choice questions (MCQs) on the Digestive System that are NCLEX-based, with detailed rationales for nursing officer exam preparation.
1. Which part of the digestive system is responsible for most of the absorption of nutrients?
- A) Stomach
- B) Large intestine
- C) Small intestine
- D) Mouth
Answer: C) Small intestine
Rationale: The small intestine is the primary site for nutrient absorption. The villi and microvilli lining the small intestine increase the surface area for absorption of nutrients such as glucose, amino acids, and fatty acids.
2. Which enzyme is primarily responsible for digesting carbohydrates in the mouth?
- A) Amylase
- B) Pepsin
- C) Lipase
- D) Trypsin
Answer: A) Amylase
Rationale: Salivary amylase, produced by the salivary glands, begins the digestion of carbohydrates in the mouth by breaking down starches into maltose.
3. What is the primary function of the pancreas in digestion?
- A) Produce bile
- B) Digest proteins
- C) Secrete digestive enzymes and bicarbonate
- D) Absorb nutrients
Answer: C) Secrete digestive enzymes and bicarbonate
Rationale: The pancreas secretes digestive enzymes (amylase, lipase, proteases) and bicarbonate to neutralize stomach acid, facilitating the digestion of carbohydrates, fats, and proteins in the small intestine.
4. Which hormone is released when food enters the stomach to stimulate gastric acid secretion?
- A) Insulin
- B) Glucagon
- C) Gastrin
- D) Secretin
Answer: C) Gastrin
Rationale: Gastrin is released by G cells in the stomach lining in response to the presence of food, which stimulates the secretion of gastric acid to aid in digestion.
5. Which of the following is a primary function of the large intestine?
- A) Nutrient absorption
- B) Bile production
- C) Water and electrolyte absorption
- D) Protein digestion
Answer: C) Water and electrolyte absorption
Rationale: The large intestine absorbs water, electrolytes, and some vitamins, and it is also involved in the formation of feces.
6. What is the role of the gallbladder in digestion?
- A) Storage of bile
- B) Secretion of digestive enzymes
- C) Production of insulin
- D) Absorption of nutrients
Answer: A) Storage of bile
Rationale: The gallbladder stores and concentrates bile produced by the liver, releasing it into the small intestine when fat is present to aid in fat digestion.
7. What is the function of the lower esophageal sphincter (LES)?
- A) Prevent reflux of stomach contents into the esophagus
- B) Aid in the absorption of nutrients
- C) Control the release of bile into the small intestine
- D) Regulate the movement of chyme into the large intestine
Answer: A) Prevent reflux of stomach contents into the esophagus
Rationale: The LES prevents the backward flow (reflux) of stomach acid into the esophagus, protecting the esophageal lining from acid damage.
8. Which structure increases the surface area for absorption in the small intestine?
- A) Rugae
- B) Villi and microvilli
- C) Pyloric sphincter
- D) Peyer’s patches
Answer: B) Villi and microvilli
Rationale: Villi and microvilli are tiny finger-like projections that line the inner surface of the small intestine, greatly increasing surface area for nutrient absorption.
9. What is the major enzyme involved in the digestion of proteins in the stomach?
- A) Amylase
- B) Pepsin
- C) Lipase
- D) Trypsin
Answer: B) Pepsin
Rationale: Pepsin is the main enzyme responsible for protein digestion in the stomach. It is activated from its inactive form, pepsinogen, in the acidic environment of the stomach.
10. Which condition is characterized by the reflux of stomach contents into the esophagus?
- A) Gastric ulcer
- B) Irritable bowel syndrome
- C) Gastroesophageal reflux disease (GERD)
- D) Crohn’s disease
Answer: C) Gastroesophageal reflux disease (GERD)
Rationale: GERD is a condition where stomach acid or contents flow back into the esophagus, causing symptoms such as heartburn and irritation of the esophageal lining.
11. Which substance is primarily absorbed in the ileum of the small intestine?
- A) Carbohydrates
- B) Proteins
- C) Water
- D) Vitamin B12 and bile salts
Answer: D) Vitamin B12 and bile salts
Rationale: The ileum absorbs vitamin B12 and bile salts, essential for red blood cell production and fat digestion, respectively.
12. Which of the following enzymes is responsible for digesting fats?
- A) Amylase
- B) Lipase
- C) Trypsin
- D) Pepsin
Answer: B) Lipase
Rationale: Lipase is the enzyme responsible for breaking down fats (lipids) into fatty acids and glycerol in the small intestine.
13. The production of bile is a function of which organ?
- A) Liver
- B) Gallbladder
- C) Pancreas
- D) Small intestine
Answer: A) Liver
Rationale: The liver produces bile, which is essential for the digestion and absorption of fats in the small intestine.
14. Which nutrient is primarily absorbed in the stomach?
- A) Proteins
- B) Carbohydrates
- C) Water and alcohol
- D) Fats
Answer: C) Water and alcohol
Rationale: The stomach primarily absorbs water and alcohol, though absorption of other nutrients occurs mainly in the small intestine.
15. The process of peristalsis is primarily responsible for which action?
- A) Mechanical digestion
- B) Chemical digestion
- C) Movement of food through the digestive tract
- D) Absorption of nutrients
Answer: C) Movement of food through the digestive tract
Rationale: Peristalsis is the wave-like muscular contractions that propel food through the digestive tract, including the esophagus, stomach, and intestines.
16. What is the major function of the mucosal lining of the stomach?
- A) Absorption of nutrients
- B) Protection against stomach acid
- C) Secretion of digestive enzymes
- D) Transport of food to the small intestine
Answer: B) Protection against stomach acid
Rationale: The mucosal lining of the stomach secretes mucus that protects the stomach lining from being damaged by the acidic environment necessary for digestion.
17. What is the role of the pyloric sphincter?
- A) Prevents bile from entering the stomach
- B) Controls the flow of food from the stomach to the duodenum
- C) Regulates the release of digestive enzymes
- D) Closes the esophagus during swallowing
Answer: B) Controls the flow of food from the stomach to the duodenum
Rationale: The pyloric sphincter regulates the passage of partially digested food (chyme) from the stomach to the duodenum of the small intestine.
18. Which of the following best describes the function of the liver in relation to nutrients?
- A) Breaks down carbohydrates
- B) Stores glycogen and regulates blood sugar
- C) Absorbs water
- D) Digests proteins
Answer: B) Stores glycogen and regulates blood sugar
Rationale: The liver stores glycogen and converts it back into glucose when blood sugar levels are low, thus regulating blood sugar levels.
19. Which part of the gastrointestinal tract is responsible for the majority of water absorption?
- A) Stomach
- B) Small intestine
- C) Large intestine
- D) Duodenum
Answer: C) Large intestine
Rationale: The large intestine is primarily responsible for absorbing water and electrolytes, which helps in the formation of solid stool.
20. Which of the following cells in the stomach secrete hydrochloric acid?
- A) Parietal cells
- B) Chief cells
- C) G cells
- D) Enterochromaffin-like cells
Answer: A) Parietal cells
Rationale: Parietal cells secrete hydrochloric acid (HCl), which helps in the digestion of proteins and kills harmful microorganisms in food.
21. What is the primary function of bile in digestion?
- A) Neutralizing stomach acid
- B) Emulsifying fats
- C) Breaking down carbohydrates
- D) Absorbing water
Answer: B) Emulsifying fats
Rationale: Bile, produced by the liver and stored in the gallbladder, emulsifies fats in the small intestine, making them easier to digest by lipase.
22. Which of the following is the most common cause of peptic ulcers?
- A) Stress
- B) Excessive alcohol consumption
- C) Helicobacter pylori infection
- D) Smoking
Answer: C) Helicobacter pylori infection
Rationale: Helicobacter pylori, a bacteria, is the primary cause of peptic ulcers, leading to the erosion of the stomach or duodenal lining.
23. What is the function of villi in the small intestine?
- A) Absorb nutrients
- B) Produce digestive enzymes
- C) Store bile
- D) Protect the intestinal lining
Answer: A) Absorb nutrients
Rationale: Villi are finger-like projections in the small intestine that increase surface area for the absorption of nutrients into the bloodstream.
24. Which hormone helps regulate the release of bile from the gallbladder?
- A) Cholecystokinin (CCK)
- B) Gastrin
- C) Insulin
- D) Secretin
Answer: A) Cholecystokinin (CCK)
Rationale: Cholecystokinin (CCK) stimulates the gallbladder to contract and release bile into the duodenum, aiding in fat digestion.
25. Which enzyme is responsible for digesting fats in the small intestine?
- A) Amylase
- B) Trypsin
- C) Lipase
- D) Pepsin
Answer: C) Lipase
Rationale: Lipase, secreted by the pancreas, is responsible for breaking down fats into fatty acids and glycerol in the small intestine.
26. What is the role of secretin in the digestive process?
- A) Stimulate pancreatic bicarbonate secretion
- B) Stimulate bile production
- C) Stimulate gastric acid secretion
- D) Increase gastric motility
Answer: A) Stimulate pancreatic bicarbonate secretion
Rationale: Secretin is released in response to acidic chyme entering the duodenum. It stimulates the pancreas to release bicarbonate to neutralize the acid.
27. Which of the following is a primary function of the stomach?
- A) Nutrient absorption
- B) Protein digestion
- C) Bile storage
- D) Water absorption
Answer: B) Protein digestion
Rationale: The stomach is primarily involved in the digestion of proteins through the action of pepsin and the acidic environment it creates.
28. What is the pH level of gastric juice in the stomach?
- A) 1.5 to 3.5
- B) 4.5 to 5.5
- C) 7 to 8
- D) 9 to 10
Answer: A) 1.5 to 3.5
Rationale: The pH of gastric juice is highly acidic, ranging from 1.5 to 3.5, which is necessary for the activation of pepsin and the breakdown of proteins.
29. Which of the following is a common symptom of gallbladder disease (cholecystitis)?
- A) Abdominal bloating
- B) Right upper quadrant pain
- C) Weight loss
- D) Dark-colored stools
Answer: B) Right upper quadrant pain
Rationale: Cholecystitis, or inflammation of the gallbladder, often causes right upper quadrant abdominal pain, especially after eating fatty foods.
30. Which of the following structures prevents the backflow of chyme from the small intestine into the stomach?
- A) Pyloric sphincter
- B) Ileocecal valve
- C) Lower esophageal sphincter
- D) Anal sphincter
Answer: A) Pyloric sphincter
Rationale: The pyloric sphincter prevents the backflow of chyme from the small intestine into the stomach and regulates the flow of chyme into the duodenum.
31. What is the primary function of the appendix?
- A) Produce bile
- B) Absorb nutrients
- C) Store beneficial bacteria
- D) Digest carbohydrates
Answer: C) Store beneficial bacteria
Rationale: The appendix is thought to serve as a storehouse for beneficial gut bacteria, aiding in the restoration of the gut microbiota after illness.
32. What condition is characterized by the chronic inflammation of the bowel, often causing abdominal pain and diarrhea?
- A) Celiac disease
- B) Irritable bowel syndrome (IBS)
- C) Crohn’s disease
- D) Gallstones
Answer: C) Crohn’s disease
Rationale: Crohn’s disease is a type of inflammatory bowel disease (IBD) that causes chronic inflammation in the gastrointestinal tract, often leading to symptoms such as abdominal pain and diarrhea.
33. Which of the following is a function of the liver?
- A) Absorb nutrients
- B) Synthesize bile
- C) Store food
- D) Neutralize stomach acid
Answer: B) Synthesize bile
Rationale: The liver produces bile, which is necessary for the digestion and absorption of fats in the small intestine.
34. Which of the following is a primary symptom of peptic ulcers?
- A) Nausea and vomiting
- B) Epigastric pain
- C) Diarrhea
- D) Jaundice
Answer: B) Epigastric pain
Rationale: Epigastric pain, often described as a burning sensation, is a hallmark symptom of peptic ulcers, typically occurring after meals or at night.
35. What is the first part of the small intestine called?
- A) Jejunum
- B) Duodenum
- C) Ileum
- D) Cecum
Answer: B) Duodenum
Rationale: The duodenum is the first part of the small intestine, where bile and pancreatic enzymes mix with chyme to continue digestion.
36. Which condition is characterized by the inflammation of the liver, commonly caused by viral infections or alcohol use?
- A) Hepatitis
- B) Cirrhosis
- C) Cholecystitis
- D) Colitis
Answer: A) Hepatitis
Rationale: Hepatitis is the inflammation of the liver, often caused by viral infections (Hepatitis A, B, C) or alcohol abuse, leading to symptoms such as jaundice and fatigue.
37. What is the primary cause of lactose intolerance?
- A) Insufficient bile production
- B) Low stomach acid
- C) Deficiency of lactase enzyme
- D) Inadequate pancreatic function
Answer: C) Deficiency of lactase enzyme
Rationale: Lactose intolerance occurs when there is a deficiency of lactase, the enzyme required to digest lactose, a sugar found in milk and dairy products.
Tag
Digestive System Notes for Nursing Officer Exam, Digestive System Anatomy and Physiology, Digestive System Nursing Notes, digestive system notes for b pharmacy, digestive system for nursing students, digestive system nurseslabs, digestive system notes for competitive exams,
Digestive System Notes for Nursing Officer Exam, Digestive System Anatomy and Physiology, Digestive System Nursing Notes, digestive system notes for b pharmacy, digestive system for nursing students, digestive system nurseslabs, digestive system notes for competitive exams,digestive system nursing notes
digestive system notes for b pharmacy
digestive system for nursing students
digestive system nurseslabs
digestive system notes for competitive exams
digestive system nursing
digestive system nursing notes pdf
digestive system nursing notes ppt
bsc nursing digestive system notes pdf download
digestive system anatomy bsc nursing 1st year notes
notes about the digestive system
****
digestive system short notes
digestive system summary notes
functions of the digestive system note guide
digestive system nursing ppt
digestive system nursing diagnosis
bsc nursing anatomy digestive system notes
notes about digestion
digestive system notes anatomy and physiology pdf
digestive system notes bsc nursing
bsc nursing digestive system notes pdf
digestive system of human notes
digestive system nursing notes, digestive system notes for b pharmacy, digestive system for nursing students, digestive system nurseslabs, digestive system notes for competitive exams, digestive system nursing, digestive system nursing notes pdf, digestive system nursing notes ppt, bsc nursing digestive system notes pdf download, digestive system anatomy bsc nursing 1st year notes,
notes about the digestive system, digestive system short notes, digestive system summary notes, functions of the digestive system note guide, digestive system nursing ppt, digestive system nursing diagnosis, bsc nursing anatomy digestive system notes, notes about digestion, digestive system notes anatomy and physiology pdf, digestive system notes bsc nursing, bsc nursing digestive system notes pdf, digestive system of human notes
Digestive System Notes for Nursing Officer Exam, Digestive System Notes for Nursing Officer Exam, Digestive System Notes for Nursing Officer Exam, Digestive System Notes for Nursing Officer Exam, Digestive System Notes for Nursing Officer Exam. Digestive System Notes for Nursing Officer Exam