Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success: The cardiovascular system is a complex organ system responsible for transporting blood, oxygen, nutrients, hormones, and waste products throughout the body. It includes the heart, blood vessels, and blood.
Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success
Heart Anatomy and Physiology
- Structure of the Heart:
- Chambers:
- Right Atrium (RA)
- Right Ventricle (RV)
- Left Atrium (LA)
- Left Ventricle (LV)
- Valves:
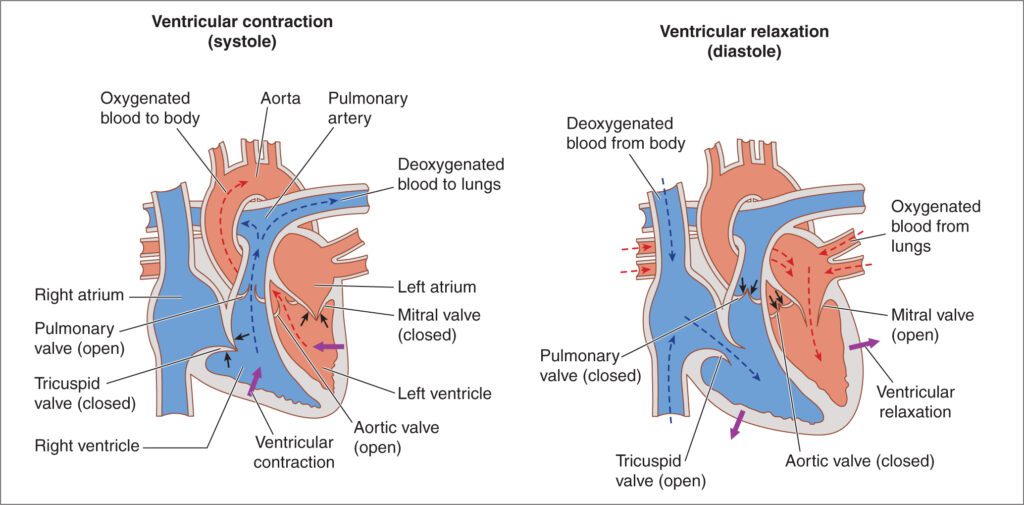
- Atrioventricular valves: Tricuspid (RA → RV) & Mitral (LA → LV)
- Semilunar valves: Pulmonary (RV → pulmonary artery) & Aortic (LV → aorta)
- Chambers:
- Layers of the Heart:
- Pericardium: Outer protective layer.
- Myocardium: Muscular middle layer, contracts to pump blood.
- Endocardium: Inner smooth layer lining the heart chambers.
- Blood Flow Pathway: Body → RA → RV → Lungs → LA → LV → Body
Oxygen-poor blood enters the RA, is pumped to the RV, and oxygenated in the lungs. It returns to the LA, moves to the LV, and is pumped throughout the body. - Conduction System:
- Sinoatrial (SA) Node: Pacemaker, generates impulses.
- Atrioventricular (AV) Node: Delays impulses for ventricular filling.
- Bundle of His and Purkinje fibers: Conduct impulses for coordinated contraction.
- Cardiac Output:
Formula: CO = HR × SV- HR (Heart Rate): Number of beats per minute (normal: 60–100 bpm).
- SV (Stroke Volume): Blood pumped per beat (~70 mL/beat).
Blood Vessels
- Arteries: Carry oxygenated blood away from the heart (except pulmonary artery).
- Veins: Return deoxygenated blood to the heart (except pulmonary vein).
- Capillaries: Facilitate gas, nutrient, and waste exchange.
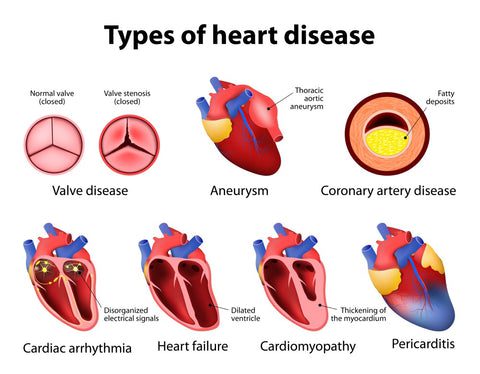
Common Cardiovascular Diseases
- Coronary Artery Disease (CAD):
- Cause: Atherosclerosis (plaque build-up in coronary arteries).
- Symptoms: Chest pain (angina), shortness of breath, fatigue.
- Complications: Myocardial infarction (heart attack).
- Hypertension (High Blood Pressure):
- Normal BP: <120/80 mmHg.
- Stages:
- Elevated: 120-129/<80 mmHg.
- Stage 1: 130-139/80-89 mmHg.
- Stage 2: ≥140/90 mmHg.
- Heart Failure:
- Types: Left-sided (pulmonary congestion), Right-sided (peripheral edema), Congestive (both).
- Symptoms: Dyspnea, edema, fatigue, reduced exercise capacity.
- Arrhythmias:
- Examples: Atrial fibrillation, ventricular tachycardia, bradycardia.
- Symptoms: Palpitations, dizziness, syncope.
- Valvular Diseases:
- Stenosis: Narrowing of valves.
- Regurgitation: Backflow of blood.
- Congenital Heart Diseases:
E.g., Septal defects, Tetralogy of Fallot. - Peripheral Artery Disease (PAD):
Affects limbs, causing pain and decreased mobility.
Cardiovascular Diseases Treatment and Medications
- Lifestyle Modifications:
- Diet: Low salt, low fat, high fiber.
- Exercise: Regular aerobic activity.
- Smoking cessation.
- Pharmacological Treatment:
- Anti-hypertensives:
- ACE inhibitors (e.g., Enalapril, Lisinopril).
- Beta-blockers (e.g., Metoprolol, Atenolol).
- Calcium channel blockers (e.g., Amlodipine).
- Diuretics (e.g., Furosemide, Hydrochlorothiazide).
- Anti-anginals: Nitroglycerin.
- Anti-arrhythmics: Amiodarone, Digoxin.
- Anti-coagulants: Heparin, Warfarin.
- Statins: Atorvastatin, Rosuvastatin (reduce cholesterol).
- Anti-hypertensives:
- Interventional Procedures:
- Angioplasty and stenting for blocked arteries.
- Coronary artery bypass grafting (CABG).
- Pacemaker insertion for arrhythmias.
- Emergency Care for Myocardial Infarction (MI):
- Immediate MONA therapy:
- Morphine for pain.
- Oxygen therapy.
- Nitroglycerin for vasodilation.
- Aspirin to prevent clot formation.
- Immediate MONA therapy:
Cardiovascular Diseases Diagnostic Tools
- Electrocardiogram (ECG/EKG): Detects electrical activity abnormalities.
- Echocardiogram: Ultrasound of the heart for structural issues.
- Blood Tests:
- Troponin levels (indicator of MI).
- Lipid profile (cholesterol levels).
- Angiography: Visualizes coronary arteries.
- Stress Testing: Evaluates cardiac performance under stress.
Important Nursing Considerations
- Monitor Vital Signs:
- BP, HR, respiratory rate, oxygen saturation.
- Assess Symptoms:
- Chest pain: Location, intensity, duration.
- Signs of fluid overload (e.g., edema, weight gain).
- Administer Medications:
- Verify correct dosage and monitor for side effects (e.g., hypotension, bleeding).
- Patient Education:
- Importance of medication adherence.
- Recognizing early signs of complications.
- Lifestyle changes to prevent disease progression.
Cardiac Cycle
The cardiac cycle refers to the sequence of events during one complete heartbeat, involving the contraction (systole) and relaxation (diastole) of the heart chambers. The cycle ensures efficient blood flow through the heart and to the rest of the body.
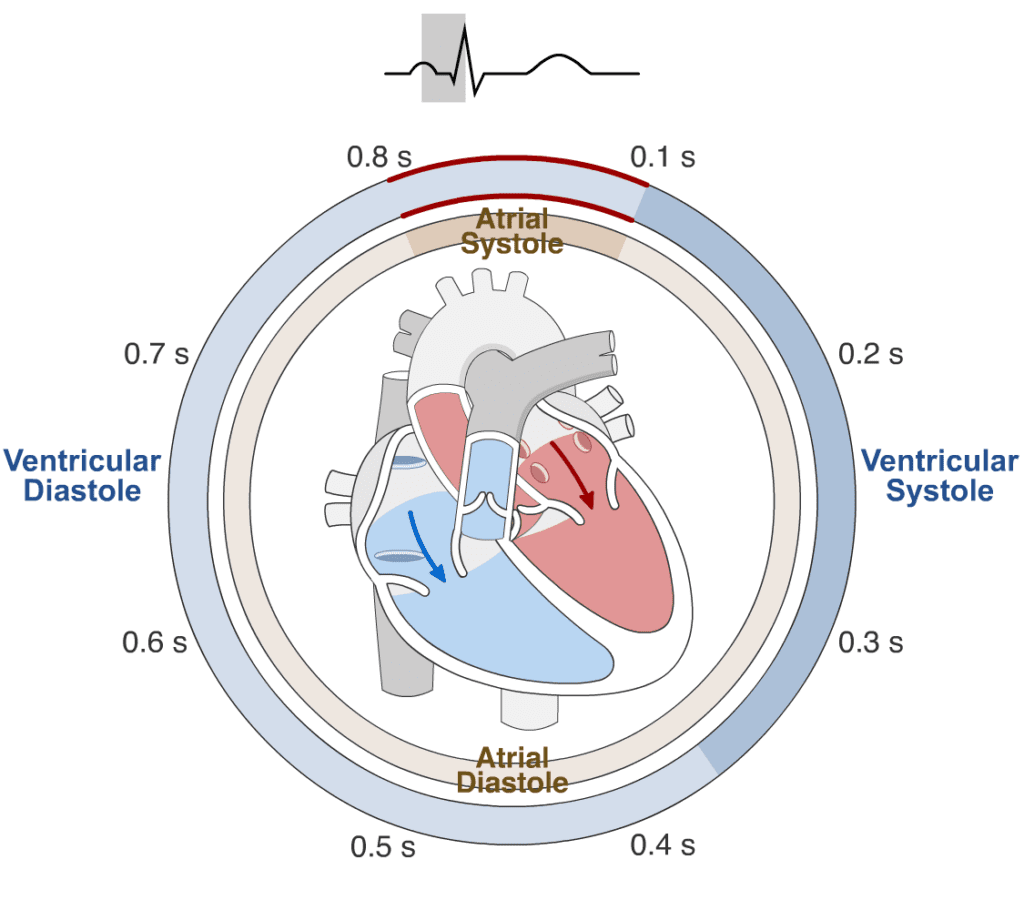
Phases of the Cardiac Cycle
- Atrial Systole (0.1 sec):
- The atria contract, pushing blood into the ventricles.
- AV valves (tricuspid and mitral) remain open.
- Semilunar valves (aortic and pulmonary) are closed.
- Ventricular Systole (0.3 sec): a. Isovolumetric Contraction:
- Ventricles contract with no volume change.
- AV valves close, producing the first heart sound (S1).
b. Ejection Phase: - Increased pressure opens semilunar valves.
- Blood is ejected into the pulmonary artery and aorta.
- Diastole (0.4 sec): a. Isovolumetric Relaxation:
- Ventricles relax, semilunar valves close, creating the second heart sound (S2). b. Ventricular Filling:
- AV valves open, and blood flows passively from atria to ventricles.
Duration of the Cardiac Cycle
- At a heart rate of 75 beats per minute, the cardiac cycle lasts approximately 0.8 seconds.
- The duration decreases with increased heart rate (e.g., during exercise).
Abnormal Heart Rhythms (Arrhythmias)
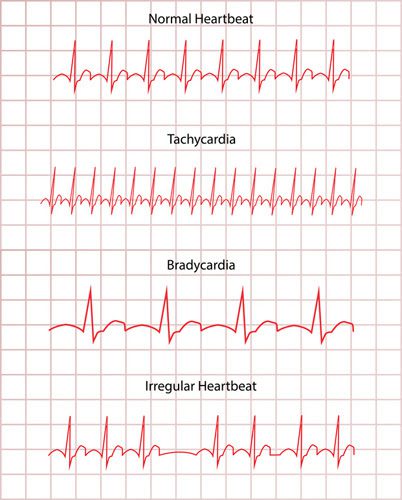
Normal Heart Rate:
- 60–100 beats per minute (bpm) at rest.
Types of Abnormal Heart Rhythms
- Tachycardia (Fast Heart Rate):
- Definition: HR >100 bpm.
- Causes:
- Exercise, fever, dehydration, stress, hyperthyroidism.
- Arrhythmias: Supraventricular tachycardia (SVT), ventricular tachycardia.
- Symptoms: Palpitations, dizziness, shortness of breath.
- Bradycardia (Slow Heart Rate):
- Definition: HR <60 bpm.
- Causes:
- Athletes (physiological), hypothyroidism, heart block.
- Symptoms: Fatigue, lightheadedness, fainting (syncope).
- Atrial Fibrillation (AFib):
- Irregular, fast atrial rhythm leading to ineffective atrial contraction.
- Causes: Hypertension, CAD, valvular heart disease.
- Complications: Stroke due to clot formation.
- Treatment: Anticoagulants (Warfarin), rate control (beta-blockers).
- Ventricular Tachycardia (VT):
- Rapid ventricular contractions.
- Life-threatening if sustained (can lead to ventricular fibrillation).
- Treatment: Cardioversion, antiarrhythmic drugs (e.g., Amiodarone).
- Ventricular Fibrillation (VF):
- Chaotic ventricular activity, no effective contraction.
- Emergency: Leads to cardiac arrest.
- Treatment: Immediate defibrillation.
- Heart Block:
- Impaired conduction between atria and ventricles.
- Types:
- First-degree: Prolonged PR interval.
- Second-degree: Intermittent conduction failure.
- Third-degree: Complete block, atria, and ventricles beat independently.
- Treatment: Pacemaker.
- Premature Contractions:
- Premature Atrial Contraction (PAC): Early atrial contraction.
- Premature Ventricular Contraction (PVC): Early ventricular contraction.
- Often benign but may indicate underlying issues.
Nursing Implications for Arrhythmias
- Assessment:
- Monitor vital signs and ECG for rhythm changes.
- Assess symptoms: Palpitations, chest pain, dizziness.
- Interventions:
- Administer medications as prescribed (e.g., beta-blockers, antiarrhythmics).
- Prepare for emergency interventions (e.g., defibrillation, pacemaker insertion).
- Patient Education:
- Importance of medication adherence.
- Recognizing signs of arrhythmia and when to seek help.
- Lifestyle changes: Avoid caffeine, alcohol, and smoking.
Top 20 MCQs on the Cardiovascular System and Diseases for Nursing Exams
1. The pacemaker of the heart is located in which part?
a) Atrioventricular (AV) node
b) Sinoatrial (SA) node
c) Bundle of His
d) Purkinje fibers
Answer: b) Sinoatrial (SA) node
Rationale: The SA node is the natural pacemaker of the heart, initiating the electrical impulse that regulates the heartbeat.
2. Which heart sound is associated with the closure of the AV valves?
a) S1
b) S2
c) S3
d) S4
Answer: a) S1
Rationale: The first heart sound (S1) is caused by the closure of the mitral and tricuspid (AV) valves during the beginning of ventricular systole.
3. What is the normal range of cardiac output in an adult?
a) 1–2 L/min
b) 4–8 L/min
c) 10–12 L/min
d) 15–20 L/min
Answer: b) 4–8 L/min
Rationale: Cardiac output, the amount of blood the heart pumps per minute, is typically 4–8 L/min in a healthy adult.
4. Which of the following is a modifiable risk factor for coronary artery disease (CAD)?
a) Age
b) Family history
c) Smoking
d) Gender
Answer: c) Smoking
Rationale: Smoking is a modifiable risk factor for CAD, whereas age, gender, and family history are non-modifiable.
5. Which ECG change is commonly seen in a myocardial infarction (MI)?
a) Prolonged PR interval
b) ST-segment elevation
c) Inverted T waves
d) Atrial fibrillation
Answer: b) ST-segment elevation
Rationale: ST-segment elevation is a hallmark sign of an acute MI, indicating myocardial injury.
6. What is the therapeutic INR range for a patient on warfarin therapy?
a) 1.0–1.5
b) 2.0–3.0
c) 4.0–5.0
d) 0.8–1.2
Answer: b) 2.0–3.0
Rationale: The therapeutic range for INR in patients on warfarin is 2.0–3.0, ensuring anticoagulation without excessive bleeding risk.
7. Which drug is the first-line treatment for acute chest pain in suspected MI?
a) Aspirin
b) Digoxin
c) Furosemide
d) Amiodarone
Answer: a) Aspirin
Rationale: Aspirin helps reduce clot formation by inhibiting platelet aggregation and is a first-line treatment in acute MI.
8. The Frank-Starling law of the heart states that:
a) Heart rate increases with sympathetic stimulation.
b) Stroke volume increases with increased end-diastolic volume.
c) Cardiac output decreases with increased preload.
d) Blood pressure is inversely proportional to cardiac output.
Answer: b) Stroke volume increases with increased end-diastolic volume.
Rationale: The Frank-Starling law explains that the heart pumps more forcefully when stretched by increased venous return (end-diastolic volume).
9. A patient with heart failure is prescribed digoxin. Which electrolyte imbalance increases the risk of digoxin toxicity?
a) Hyperkalemia
b) Hypokalemia
c) Hypercalcemia
d) Hyponatremia
Answer: b) Hypokalemia
Rationale: Low potassium levels enhance digoxin’s effect, increasing the risk of toxicity.
10. Which type of shock is caused by a massive myocardial infarction?
a) Cardiogenic shock
b) Hypovolemic shock
c) Septic shock
d) Neurogenic shock
Answer: a) Cardiogenic shock
Rationale: Cardiogenic shock occurs when the heart cannot pump effectively, often due to a large MI.
11. The normal range for ejection fraction (EF) in a healthy heart is:
a) 20–40%
b) 50–70%
c) 30–50%
d) 10–30%
Answer: b) 50–70%
Rationale: Ejection fraction measures the percentage of blood pumped out of the ventricles and is typically 50–70% in a healthy heart.
12. Which medication class is commonly used to treat hypertension and heart failure?
a) Beta-blockers
b) NSAIDs
c) Antihistamines
d) Antibiotics
Answer: a) Beta-blockers
Rationale: Beta-blockers reduce blood pressure and heart workload, making them useful for hypertension and heart failure.
13. What is a common cause of sudden cardiac arrest in adults?
a) Hypertension
b) Coronary artery disease
c) Hyperthyroidism
d) Atrial fibrillation
Answer: b) Coronary artery disease
Rationale: CAD can lead to ventricular fibrillation, the most common cause of sudden cardiac arrest.
14. Which test is most specific for diagnosing an acute myocardial infarction?
a) CK-MB
b) Troponin I or T
c) LDH
d) ECG
Answer: b) Troponin I or T
Rationale: Troponins are cardiac-specific biomarkers with high sensitivity and specificity for detecting myocardial infarction.
15. Which condition is characterized by a narrowed pulse pressure?
a) Hypotension
b) Cardiac tamponade
c) Atrial fibrillation
d) Hypertension
Answer: b) Cardiac tamponade
Rationale: Cardiac tamponade restricts ventricular filling, leading to a narrowed pulse pressure.
16. Which of the following is NOT a symptom of heart failure?
a) Dyspnea
b) Peripheral edema
c) Hemoptysis
d) Fatigue
Answer: c) Hemoptysis
Rationale: Hemoptysis is not a common symptom of heart failure; dyspnea, edema, and fatigue are typical.
17. Which antihypertensive is contraindicated in pregnancy?
a) Labetalol
b) Methyldopa
c) ACE inhibitors
d) Hydralazine
Answer: c) ACE inhibitors
Rationale: ACE inhibitors are teratogenic and contraindicated during pregnancy.
18. What is the target LDL cholesterol level in patients with cardiovascular disease?
a) <100 mg/dL
b) <130 mg/dL
c) <160 mg/dL
d) <190 mg/dL
Answer: a) <100 mg/dL
Rationale: In patients with CVD, LDL cholesterol should be maintained below 100 mg/dL to reduce cardiovascular risk.
19. Which heart rhythm is characterized by a sawtooth pattern on ECG?
a) Atrial fibrillation
b) Atrial flutter
c) Ventricular tachycardia
d) Second-degree heart block
Answer: b) Atrial flutter
Rationale: Atrial flutter presents as a sawtooth pattern due to rapid, regular atrial contractions.
20. Which drug is used as a thrombolytic agent in acute MI?
a) Streptokinase
b) Aspirin
c) Nitroglycerin
d) Clopidogrel
Answer: a) Streptokinase
Rationale: Streptokinase is a thrombolytic agent that dissolves blood clots in acute MI.
Tags
cardiovascular system, nursing exams, heart diseases, cardiac cycle, abnormal heart rhythms, heart anatomy, cardiovascular physiology, coronary artery disease, ECG interpretation, myocardial infarction, heart failure, blood circulation, nursing study materials, cardiovascular treatments, cardiac drugs, nursing MCQs, cardiac nursing care, nursing exam preparation, cardiovascular pathology, heart medications, Cardiovascular System, Cardiovascular System, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success
comprehensive guide to the cardiovascular system for nursing exams, master cardiovascular nursing concepts, study materials and MCQs, top nursing exam questions on heart diseases and treatments, learn the cardiac cycle and abnormal heart rhythms easily, essential cardiovascular system study guide for nurses, heart diseases explained tips for nursing exam success, cardiovascular pathology simplified for nursing students, prepare for nursing exams with cardiac drug insights, detailed cardiovascular system notes for nurses, crack nursing exams focus on cardiovascular health, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success
Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success, Cardiovascular System: Nursing Exam Prep Notes & Top 20 MCQs for Success